The Faculty of Allied Health Sciences, Thammasat University conducted research on “Innovation of Monoclonal Antibodies Production to the Dia blood type by Phage Display Technology” where the research team was led by Prof.Maj. Gen. Dr. Oytip Nathalang, Director of Graduate Programs and Asst.Prof.Dr. Jeeraphong Thanongsaksakul, Assistant Dean for Administration and Head of the Molecular Diagnosis Laboratory, Health Care Service Center, Faculty of Allied Health Sciences, TU.
This technology is the production of “Antibody to specific blood type” that allows the test of an important blood type in Thailand and Asian populations, which is Dia (Diego a), to be more accurate and to prepare safe blood and blood products for patients who require regular blood transfusions.
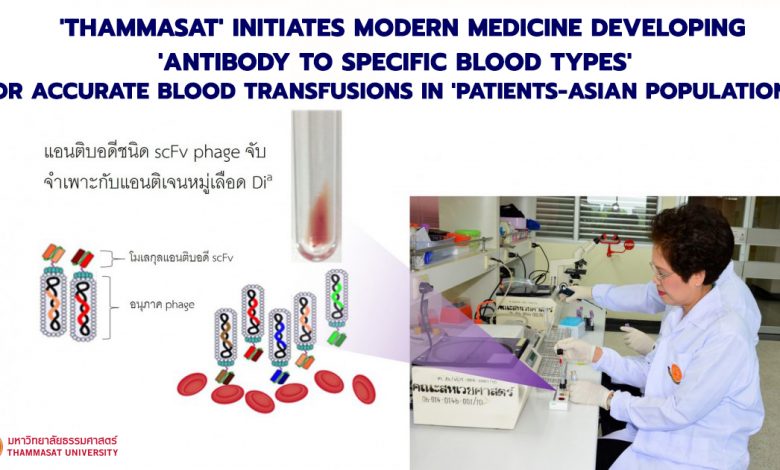
Asst. Prof. Dr. Jeeraphong explained that the technology is initiated to simulate the mouse antibody library in vitro by Phage Display Technology which antibody genes are deposited into bacterial viral particles called “phages”. Each phage particle acts as a white blood cell to hold an antibody molecule on the particle surface with a variety of antibodies, which is called “antibody-phage library“.
“If antibodies to Dia blood type is required, we just simply match red blood cell molecules containing this blood type with a phage that have the antibody molecule on the particle surface of the specific Dia blood type. Consequently, specific antibodies will be selected to increase the amount of antibodies attached to phage particles in bacterial cells to be sufficient for testing for specificity of Dia blood type by a biotechnological process,”said Asst.Prof.Dr. Jeeraphong.
In addition, the method used by the Faculty of Allied Health Sciences, Thammasat University has a procedure to remove antibodies specific to other important and common blood types in Thai population in order to increase the specificity of the production of antibodies against Dia blood type.
Asst.Prof.Dr. Jeeraphong explained that currently the reagents used to test the Dia blood group must be imported. It is produced from the separation of lymph from the blood of people who produce antibodies to the Dia blood group.
“Each batch of the imported reagent is probably obtained from the same donor but at different times of collection or from different donors. This resulted in lot-to-lot variation because the antibodies produced in the human body vary according to the environmental response. However, the production of antibodies against Dia blood group that the Faculty of Allied Health Sciences, Thammasat University uses is a technique that produces antibodies in vitro with Phage Display Technology. Thus, the quality of antibodies in each batch is more stable,” Asst.Prof.Dr. Jeeraphong said
In addition, the Faculty of Allied Health Sciences, Thammasat University has signed an agreement and transferred technology knowledge with a biotechnology company in Germany in order to develop antibodies against Dia blood group that the Faculty of Allied Health Sciences, Thammasat University has produced to be suitable for use in daily diagnostic tests or in automated analyzers for further commercial reason.
“When TU passes on the prototype to them, they must develop it into an acceptable form as a medical device. If the development process is successful, the agreement we have signed will reach the commercial objective and if the formula works well, it can be sold which will allow patients to get an access to reagents and more accurate test that patients will be able to receive the matching blood group. This will reduce the side effects caused by the mismatch of blood,” Asst.Prof.Dr. Jeeraphong said.
Asst.Prof.Dr. Jeeraphong explained further that the production of antibodies benefited patients requiring surgery and blood to support the symptoms – life while losing blood during surgery. But for the group that will receive benefit the most is those who regularly require blood transfusions, such as, thalassemia patients because these patients are at high risk of getting a foreign blood type from each blood transfusion. If the blood group mismatch occurs, it may stimulate the immune system to reject. However, having accurate and easily accessible blood grouping reagents will help reduce the risk for such patients.